Abstract
Purpose of review Gout is a true crystal deposition disease, extremely painful and bone and tissue damaging if untreated. It is the only curable form of arthritis. Although we have many treatments to cure gout, it is a disease that is consistently undertreated/mismanaged and perceived by clinicians and the lay public as a 'laughable condition' with the patients' lifestyle often held erroneously to account. This article would give you a good understanding of modern and established pharmacological and nonpharmacological treatments used in the management of acute and chronic gout and how to 'treat to target' to cure the disease.
Recent findings Many of the drugs we use to manage patients with gouty arthritis have been in existence since the 1970s and 1980s. In the past few years, because of the improved physiological understanding of gout, new innovative treatments such as anti-IL inhibitors, a nonxanthine oxidase inhibitor and the uricase enzymes have been developed adding to our armamentarium of drugs.
Summary With the introduction of new research, we have been able to explore how to also use established treatments more effectively, raising the profile of gout and its best management and introducing the principle of treating the patient to urate target.
Introduction
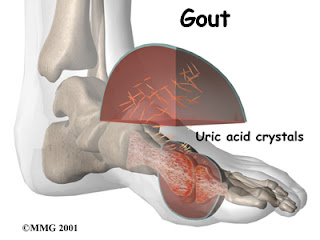
Gout is a true crystal deposition disease [monosodium urate (MSU) crystals] and the commonest inflammatory arthritis in men over the age of 40. It is the only curable form of arthritis. First identified by the Egyptians in 2640 BC, it is recognized as one of the oldest medical conditions. The UK prevalence is 1.4% which does not appear to be rising.[1,2]
Improved understanding of the pathophysiology of urate including intracellular events and renal handling in hand with the identification of many genetic components of patients with gout has helped facilitate new therapeutic modalities from bench to bedside. They have also enabled older treatment modalities to be included in contemporary research trials giving more detailed analysis of their use in modern day life with the increased comorbidities experienced by many patients with gout. Epidemiological studies on lifestyle components have similarly added to treatment options for patients giving choice. Importantly, those patients who are unable to take or are unresponsive to traditional treatments can be more adequately treated with alternative drugs and modify lifestyle, reducing treatment-resistant gout and helping minimize flare of gout on introduction of uratelowering treatments.
Unfortunately, although an ancient disease, gout is consistently poorly managed by primary and secondary care clinicians, perhaps because of initiation of treatment by nonspecialists in the majority of diagnosed cases. With the advent of newer, more expensive treatments raising the profile of gout, there may be a move back towards more specialist care thereby optimizing treatment and enabling cure for more patients.
In order to improve patient care amongst specialists and nonspecialists, guidelines have been developed by the British Society of Rheumatology (BSR)[3] and the European League against Rheumatology (EULAR).[4] These give pragmatic guidance but require updating in light of newer treatment modalities emerging.
This review aims to update the reader of recent evidence-based additions to treatment, adding to previously published British and European guidance.
Management: Lifestyle Factors
Modifications of lifestyle and diet are key components of gout management. Obesity is the commonest comorbid risk factor for gout,[1] highlighting the need to address over-weight in every patient's management plan.
Numerous previous epidemiological studies[5–7] have highlighted links with a variety of food and drinks being either protective (coffee, dairy products, and low BMI) or causative (beer, meat and seafood, and fructose) in patients with gout and are outlined in various review articles.
A recent, randomized, crossover trial[8] explored the effect of dairy products in more detail by studying the effect of drinking milk (cow and soy) on serum urate concentrations. They found intact cows milk (not soy) decreased serum urate by 10% after a 3-h follow-up period. A follow-up controlled trial[9••] by the same authors has suggested that skimmed milk enriched with glycomacropeptide or milk fat extract significantly reduces the risk of gout flare. Furthermore, a meta-analysis[10] has confirmed that supplementation with vitamin C significantly reduces serum urate levels. Further study is required, but this may suggest dairy products and vitamin C have a longer term role in the nonpharmacological management of gout patients.
In terms of increasing risk, a study[11] implicated beer consumption (but not wine) associated with elevated serum urate levels, women more so than men. Also, replicating previous observations seen in men, the NHANES study[12]confirmed women also have a higher risk of incident gout associated with consumption of fructose-rich beverages. Avoidance/reduction advice can be confidently included in patient consultation and written educational material.
Although adhering to lifestyle advice alone cannot reduce very high levels of serum urate, modification of lifestyle/diet can have a small uratelowering effect and carry additional benefits in terms of overall health, particularly with regard to the metabolic syndrome. Additionally, it provides patients with a degree of autonomy over their disease and choice of adopting lifestyle advice to manage their condition in the first instance.
Further treatment can be divided into the acute and chronic management of gout.
Acute Treatment
The main aim of acute treatment is to provide rapid relief of pain and inflammation and exclude joint sepsis. Without acute treatment, the pain from an attack can last at least a week. Time from treatment to termination of attack is the only guide to efficacy as few placebo-controlled trials exist.
In addition to pharmacological agents, affected joints should be rested and treated with ice, which has a significant anti-inflammatory effect additionally.[13]
A systematic review looked at pharmacological treatments for acute gout.[14] Only 26 suitable studies and three abstracts papers were identified demonstrating the lack of published evidence in acute management strategies. The review concluded nonsteroidal anti-inflammatory drugs (NSAIDs) and colchicine are the most frequently used effective treatments, but steroid and anti-IL-1 can be used in those who are treatment resistant.
Nonsteroidal Anti-inflammatory Drugs
NSAIDs are the most commonly used first-line treatment. Head-to-head studies show few differences between drugs.[15] Full doses of NSAID should be initiated immediately and tapered after resolution of symptoms.[3,4]
NSAIDs have numerous adverse effects and should be avoided in gastrointestinal ulcer disease, bleeding or perforation, renal insufficiency, heart failure and those taking oral anticoagulants. Adverse events are increased in the elderly and co-administration of a proton pump inhibitor should be considered. When contemplating NSAIDs, premorbid conditions and drug history should be taken into account on an individual patient basis and any current national guidance adhered to.
Colchicine Colchicine is an old-fashioned drug with modern pathophysiological effects derived from the autumn crocus. It blocks microtubule assembly in neutrophils reducing phagocytosis and transport of MSU crystals.[15] It also affects neutrophil migration into joints by reducing adhesion molecules on endothelial cells and neutrophils in response to IL-1 or TNF-a.[16] More recently, it has been demonstrated that colchicine also reduces NALP3 inflammasome-driven caspase-1 activation by microtubule inhibition which decreases MSU delivery.[15]
A RDBPCT compared colchicine low dose (1.8mg over 1 h) and high dose (4.8mg over 6 h) with placebo in 184 patients with acute gout. Low dose was as effective as high dose and both significantly more effective than placebo. The low-dose group had an adverse side-effect profile similar to placebo.[17] This suggests low-dose colchicine can be utilized effectively and safely in acute gout flare. Further dosing regimes are suggested by the BSR and EULAR.[3,4]
Adverse events of colchicine include abdominal cramps, nausea, vomiting and rarely bone marrow suppression, neuropathy and myopathy. Colchicine has the narrowest therapeutic window of any gout therapy. Reduced dosing in elderly or those with renal or hepatic impairment is imperative. Colchicine is metabolized by CYP3A4 and excreted by p-glycoprotein. Toxicity can be caused by drugs interacting with its metabolism and clearance, which include macrolides, cyclosporin and protease inhibitors.[18] Unpublished data from healthy individuals highlight the important interaction between colchicine and clarithromycin, which increases the plasma elimination half-life of colchicine by 233% via p-glycoprotein inhibition.[19] Intravenous colchicine is no longer licensed in the UK and many clinicians advocate an outright ban as it has a 2% mortality rate. No trials have directly compared NSAIDs and colchicine.
Corticosteroids Corticosteroids act on the cytosolic glucocorticoid receptor to alter gene expression. Steroids also have nongenomic effects mediated by the cytosolic glucocorticoid receptor, membrane-bound glucocorticoid receptor and additional interactions with cellular membrane proteins.[20]
In gout, corticosteroid can either be given intraarticularly (preferred route if one or two joints affected), orally, intramuscularly or intravenously. Corticosteroids are a good alternative where NSAID and colchicine cannot be used or in refractory cases. A Cochrane review demonstrated equal efficacy between corticosteroid and comparator (NSAID), but commented the studies were of poor-to-moderate quality with numerous types of active comparator making comparison difficult. There were no reported side-effects with short-term use of corticosteroid however.[21]
Anti IL-1 Therapy Blocking IL-1 is a novel concept in the treatment of acute gout but highly effective. The rationale stems from the discovery that MSU crystals stimulate the inflammasome in gout leading to IL-1b secretion.[22] In current experiments, IL-1 inhibitors prevent IL-1 secretion via this mechanism and also block IL-1 secretion by macrophages via a toll-like receptor-dependent mechanism.[23]
The anti-IL-1 drugs anakinra, canakinumab and rilonacept have all been studied in patients with acute gout.
A case report[22] and an open-labelled pilot study[23] have shown subcutaneous injections of anakinra 100mg daily to be a well tolerated and efficacious treatment of flares. Ten patients featured in the open-label study were unable to take other gout medications because of renal impairment, allergies, gastrointestinal haemorrhage and history of renal stones. Pain decreased by 79% on average after three injections.[23] No side-effects were noted during the trial, and clinical examination showed complete resolution in 9 of 10 patients on day 3.
Phase III studies have been completed using both canakinumab and rilonacept in the management of acute gout flare. In two 12 week trials (b-relieved and b-relieved II), 416 gouty arthritis patients in flare were randomized to either canakinumab 150mg subcutaneously or triamcinolone acetate 40mg intramuscularly. Superiority was significantly demonstrated over triamcinolone acetate at 12 weeks. A total of 317 patients then completed a 12-week extension study. Over the full 24-week study period, canakinumab delayed time to new flare with risk reduction of 52% (b-relieved) and 60% (b-relieved II), respectively, compared with triamcinolone acetate.[24] In the same patient population, inflammation markers (CRP and SAA) and joint tenderness and swelling were significantly diminished by 24 h as compared with triamcinolone acetate and response was sustained.[25]
In a pooled analysis of one phase II and three phase III RDBPCTs, weekly subcutaneous injection of rilonacept 80mg (n = 162) or 160mg (n = 1191) or placebo (n = 533) was given in patients at risk of flare on initiation of urate-lowering therapy (ULT). The study period was 16 weeks and assessed the side-effects. The rate of serious infections was low, with site reaction the most common adverse event, mainly in the high-dose rilonacept group.[26]The three phase III study results were then pooled to assess prevention of gout flare on initiation of ULT. Rilonacept 160 and 80mg resulted in a 69.2 and 62.3% reduction in rate of gout flare, respectively, as compared with placebo.[27]
Anti-IL-1 treatments are highly effective in terminating de novo flares in those unresponsive to NSAID and colchicine and also reducing the risk of flare on initiation of ULT; the effect is long lasting over several weeks. However, they are extremely expensive when compared with traditional acute treatment modalities, and therefore their place in management is still to be determined.
Chronic Treatment
The main aims of chronic treatment are to
- prevent recurrent attacks by using ULT and thereby alleviate complications of chronic gouty arthritis;
- 'treat to target' to prevent MSU crystal saturation and dissolve crystals already deposited in joints and soft tissue by reducing serum urate effectively (BSR <0.3 mmol/l; EULAR <0.36mmol/l);
- assess and modify contributing risk factors [e.g. hypertension, diabetes mellitus, hyperlipidaemia, heart failure, obesity, osteoarthritis, drugs (diuretics and ciclosporin)];
- provide long-term follow-up and monitoring of gout including serum urate (sUA) checks.
Complications of gout are as follows:
- tophi and soft tissue damage;
- erosive bone damage;
- renal disease:
- uric acid calculi;
- chronic urate nephropathy;
- acute uric acid nephropathy (usually secondary to chemotherapy);
- disability and work absence;
- avascular necrosis of the femoral head.
ULTs can be divided into uricostatic agents that decrease sUA production, uricosuric agents that increase renal excretion or uricolytic agents that metabolize sUA.
Uricostatic Agents: Xanthine Oxidase Inhibitors
Allopurinol Since the 1970s, allopurinol has been the mainstay of chronic treatment. It reduces sUA by inhibiting xanthine oxidase preventing xanthine being converted to uric acid. The most commonly used dose is 300mg daily, with the maximum dose of 900mg daily. However, it is thought introducing allopurinol at a dose of 100mg daily and increased by 100mg titrated against sUA and creatinine clearance may reduce flare on initiation.[3,4] Additionally, commencing at a low dose and slowly incrementing can reduce the risk of allopurinol hypersensitivity reaction.[28]
Adverse events of allopurinol include rash (2%), vasculitis, eosinophilia, life-threatening hypersensitivity reaction, hepatitis, decreased renal function and bone-marrow suppression. Allopurinol requires reduced dosing in renal impairment, this being its route of excretion.
Febuxostat Febuxostat is a new nonpurine selective xanthine oxidase inhibitor. It is a potent hypouricaemic agent primarily metabolized in the liver and therefore no dose reduction in moderate renal function is required.
A Phase 3 trial compared febuxostat 80 and 120mg with allopurinol 300mg for 52 weeks with the same sUA target.[29] The largest reduction in sUA was achieved in those receiving febuxostat 120mg (P<0.001); however, more patients in this group discontinued treatment (P<0.003). The primary end-point was reached in 53% of the patients on 80mg of febuxostat, 62% on 120mg of febuxostat and only 21% in those receiving allopurinol. However, overall rates of discontinuation were higher in both the groups of patients on febuxostat, most commonly because of deranged liver function tests (LFTs) or acute flares.
Results from a 5-year febuxostat trial[30] provide longer term safety and efficacy results.
At 5 years, 93% of the patients achieved the target of sUA less than 6.0 mg/dl with daily doses between 40 and 120 mg. Twenty-two percent (n = 26) had palpable tophi and the majority resolved. Efficacy in renal impairment was demonstrated with no significant relationship between renal function and urate-lowering efficacy found. The most common adverse event leading to withdrawal from the study was reversible LFT derangement. However, the exclusion criteria of not prescribing in patients consuming over 14 alcoholic drinks a week must be noted. The most frequently encountered serious adverse event was atrial fibrillation, but this was not attributed to febuxostat.
It is difficult to make a direct comparison on the efficacy of febuxostat in comparison with allopurinol because of the doses used and lack of escalation above 300mg allopurinol daily. Its place in treatment should be as a second-line agent where allopurinol has failed to reduce sUA or contraindicated.
Uricosuric Agents
These drugs enhance the renal clearance of urate. They are utilized much less frequently than xanthine oxidase inhibitors and are largely ineffective in patients with renal insufficiency (except benzbromarone) and should not be used in patients with nephrolithiais.
Benzbromarone Benzbromarone is metabolized by cytochrome P450 and was withdrawn from widespread use because of hepatic toxicity. It can now be used on a named patient basis in much of Europe. It is a highly effective drug at reducing sUA levels and can be used in patients with renal transplant and in combination with xanthine oxidase inhibitors.
The most recent randomized controlled trial assessing benzbromarone compared it with probenecid in patients who could not tolerate allopurinol or failed to achieve sUA of less than 0.30 mmol/l on allopurinol.[31] Twenty-four percent of the patients were successfully treated with allopurinol 300 mg/day within 2 months. In those who failed on allopurinol and were assigned to the benzbromarone (200mg once daily) arm, 92% (n = 24) achieved the sUA target compared with 65% (n = 31) in the probencid 1 g twice a day arm.
Sulphinpyrazone Sulphinpyrazone inhibits prostaglandin synthesis much like the NSAIDs and therefore its adverse events are similar including gastrointestinal ulceration, acute renal failure, fluid retention and rarely elevation of liver enzymes and blood disorders. Daily divided doses of 200–800mg are given.
Probenecid Probenecid can be effective as an add-in therapy when allopurinol alone is insufficient, but is ineffective in renal impairment. Divided doses of 0.50– 2.0 g are used, but it is rarely utilized because of difficulties with supply.
Lesinurad Lesinurad (RDEA594) is a novel uricosuric agent and has been studied in combination with allopurinol in allopurinol refractory gout patients in a phase II dosing study using 200, 400 or 600mg lesinurad plus a stable dose of allopurinol. Reduced sUA and increased response rates occurred in a doserelated manner when lesinurad was combined with allopurinol, and the findings were highly statistically significant at all combination doses when compared with allopurinol plus placebo. Lesinurad was also well tolerated.[32••] Further studies are required to explore this drug as mono and combination therapy.
Uricolytics
The human uricase gene underwent two separate mutations that independently resulted in truncation of gene transcription. This decreased uricase function, but may have increased antioxidant activity, increased intelligence and improved the ability of humans to retain salt.[33] The action of uricase converts urate to allantoin, which is 10 times more soluble and thus more readily excreted.
Rasburicase In 1996, rasburicase was developed by recombinant DNA technique from a genetically modified strain of Saccharomyces cerevisiae. The efficacy of rasburicase in prevention and treatment of tumour lysis syndrome (TLS) has been well demonstrated despite its cost.[34] However, allergenicity and development of antibodies compromise its effectiveness, the risk of which increases with repeated use.[34] Rasburicase is given intravenously at a dose of 0.20 mg/kg for 5–7 days to treat TLS. No trials have assessed rasburicase efficacy in gout, but a small study[35] compared monthly and daily regimes.
After 6 monthly infusions, sUA decreased from 612.6–162.4 mmol/l at baseline to 341.2– 91.8mmol/l (P = 0.001). Daily infusions did not produce a significantly sustained reduction, and the incidence of hypersensitivity was higher in the once daily group.
Poly(ethylene) Glycol-uricase PEGylation forms a covalent link between a protein and PEG, and has the advantageous properties of prolonging the drug half-life and decreasing antigenicity.[34] The mean termination half-life of PEG-uricase is 2 weeks compared with 19 h for rasburicase.
PEG-uricase is better tolerated intravenously than by subcutaneous injection, and postinfusion uricase activity increases in a linear fashion up to 8mg.[36] Phase 1 trials demonstrated that intravenous administration is superior to subcutaneous administration in achieving more rapid, significant and prolonged lowering of sUA.[36] PEG-uricase reduces or eliminates uric acid excretion, which is an attractive property potentially benefiting patients with uric acid nephrolithiasis. Phase 2 trials from 2004 to 2005 showed that the most effective dose is 8mg every 2 weeks, and the detection of antibodies against PEG-uricase does not appear to limit treatment either by increasing drug clearance, neutralizing treatment, or increasing adverse events.[37] If antibodies limit the efficacy of PEG-uricase, then a next generation could be developed with different coupling of uricase to PEG.
Two placebo-controlled, randomized trials in gouty patients who have failed conventional treatment are reported totalling 225 patients. Pooled results demonstrate pegloticase 8mg each fortnight and monthly, respectively, resulted in reducing sUA less than 0.36 mmol/l in 42 and 35% of patients, respectively. No patients in the placebo arm reached the endpoint.[38]
The most common adverse event of PEG-uricase is inducing an acute flare and infusion reactions. Infusion-related events included nausea, vomiting, dizziness, respiratory symptoms, myalgias and rash, but not anaphylaxis.[36]
PEG-uricase is another potentially powerful agent for treating refractory gout in those who are unable to tolerate other treatments and could have a role in 'debulking' tophi in advanced gout before switching to another agent for maintenance treatment.
Conclusion
There have been many innovations in treatment for patients with gout over recent years with additional new drugs currently in development that will help in the management of treatment resistant gout. This has raised the profile of gout as a disease entity and highlighted the current poor management experienced by many patients.
The concept of treat-to-target has been established with clear serum urate cut off, enabling practitioners and their patients to monitor treatment successfully.
Increased research into health-related quality of life for gout sufferers demonstrates a definite need for better care and if provided, clearly shows health improves.[39]
However, the main barrier to more successful treatment is altering the image of gout as a purely acute disease that is humorous and educating fellow healthcare professionals and patients to utilize the treatment armamentarium we already have available optimally.
References
- Annemans L, Spaepen E, Gaskin M, et al. Gout in the UK and Germany: prevalence, comorbidities and management in general practice 2000–2005. Ann Rheum Dis 2008; 67:906–966.
- Mikuls TR, Farrar J, Bilker WB, et al. Gout epidemiology: results from the UK general practice research database, 1990–1999. Ann Rheum Dis 2005; 64:267–272.
- Jordan KM, Cameron JS, Snaith M, et al. British Society for Rheumatology and British Health Professionals in Rheumatology guidelines for the management of gout. Rheumatology 2007; 46:1372–1374.
- Zang W, Doherty M, Bardin T, et al. EULAR evidence based recommendations for gout. Part II. Management. Report task force of the EULAR standing committee for international clinical studies including therapeutics (ESCISIT). Ann Rheum Dis 2006; 65:1312–1324.
- Rider TG, Jordan KM. The modern management of gout. Rheumatology 2010; 49:5–14.
- Singh JA, Reddy SG, Kundukulam J. Risk factors for gout and prevention: a systematic review of the literature. Curr Opin Rheumatol 2011; 23:192–202, 1531–6963.
- Li S, Micheletti R. Role of diet in rheumatic disease. Rheum Dis Clin North Am 2011; 37:119–133.
- Dalbeth N, Wong S, Gamble GD, et al. Acute effect of milk on serum urate concentrations: a randomised controlled crossover trial. Ann Rheum Dis 2010; 69:1677–1682.
- Dalbeth N, Ames R, Gamble G, et al. Daily intake of skim milk powder enriched with glycomacropeptide and G600 milk fat extract may reduce frequency of gout flares; results from a randomized, controlled trial. In: ACR Conference Proceedings; abstract 207; 2011.
••The first reported trial of a dietary intervention reducing urate levels. - Juraschek SP, Miller ER 3rd, Gelber AC. Effect of oral vitamin C supplementation on serum uric acid: a meta-analysis of randomized controlled trials. Arthritis Care Res 2011; 63:1295–1306.
- Gaffo AL, Roseman JM, Jacobs DR Jr, et al. Serum urate and its relationship with alcoholic beverage intake in men and women: findings from the Coronary Artery Risk Development in Young Adults (CARDIA) cohort. Ann Rheum Dis 2010; 69:1965–1970.
- Choi HK, Willett W, Curhan G. Fructose rich beverages and risk of gout in women. JAMA 2010; 304:2270–2278.
- Schlesinger N. Response to application of ice may help differentiate between gouty arthritis and other inflammatory arthritides. J Clin Rheumatol 2006; 12:275–276.
- Khanna P, Singh MK, Fitzgerald JD, et al. Pharmacological treatment of acute gout: a systematic review. In: ACR Conference Proceedings, abstract 1025; 2011.
- Cronstein BN, Terkeltaub R. The inflammatory process of gout and its treatment. Arthritis Res Ther 2006; 8:S1.
- Choi HK, Mount DB, Reginato AM. Pathogenesis of gout. Ann Intern Med 2005; 143:499–516.
- Terkeltaub R, Furst DE, Bennett K, et al. High versus low dosing of oral colchicine for early acute gout flare: twenty-four-hour outcome of the first multicenter, randomized, double-blind, placebo-controlled, parallel-group, dose-comparison colchicine study. Arthritis Rheum 2010; 62:1060–1068.
- Van der Velden W, Hussen J, ter Laak H, de Sevaux R. Colchicine-induced neuromyopathy in a patient with chronic renal failure: the role of clarithromycin. J Med 2008; 66:204–206.
- Terkeltaub R, Furst D, DiGiacinto J, et al. A one sequence, two-period pharmacokinetic drug-drug interaction study with colchicine reveals profound effects of clarithromycin (a macrolide antibiotic) on the pharmacokinetic profile of colchicine in healthy adults. In: ACR Conference Proceedings; abstract 1946; 2008.
- Stahn C, Löwenberg M, Hommes DW, Buttgereit F. Molecular mechanisms of glucocorticoid action and selective glucocorticoid receptor agonists. Mol Cell Endocrinol 2007; 15:71–78.
- Janssens HJ, Lucassen PLBJ, Van de Laar FA, et al. Systemic corticosteroids for acute gout. Cochrane Database Syst Rev 2008; Issue 2. Art. No. CD005521.
- McGonagle D, Tan AL, Shankaranarayana S, et al. Management of treatment resistant inflammation of acute on chronic tophaceous gout with anakinra. Ann Rheum Dis 2007; 66:1683–1684.
- So A, De Smedt T, Revaz S, Tschopp J. A pilot study of IL-1 inhibition by anakinra in acute gout. Arthritis Res Ther 2007; 9:R28.
- Brown JP, So A, Dikranian A, et al. Long-term efficacy and safety of canakinumab versus triamcinolone acetonide in acute gouty arthritis patients. In: ACR Conference Proceedings; abstract 1016; 2011.
- So A, Alten R, Schumacher HR, et al. Inflammation suppression over 24 weeks in patients with gouty arthritis: results from two phase-III core and extension studies comparing canakinumab with triamcinolone acetonide. In: ACR Conference Proceedings; abstract 1019; 2011.
- Terkeltaub R, Schumacher HR, Mitha E, et al. Integrated safety analysis of four trials of interleukin-1 blockade with rilonacept for gout flare prevention in patients taking uric acid-lowering therapy. In: ACR Conference Proceedings; abstract 1015; 2011.
- Schumacher HR, Evans RR, Birbara CA, et al. Rilonacept for prevention of gout flares associated with uric acid-lowering therapy: response rate across three phase 3 clinical trials. In: ACR Conference Proceedings; abstract 1024; 2011.
- Stamp LK, Taylor W, Jones PBB. Starting dose, but not maximum maintenance dose, is a risk factor for allopurinol hypersensitivity syndrome: a proposed nomogram for safe starting dosing of allopurinol. In: ACR Conference Proceedings; abstract 2579; 2011.
- Becker MA, Schumacher HR, Wortmann RL, et al. Febuxostat compared with allopurinol in patients with hyperuricemia and gout. N Engl J Med 2005; 353:2450–2461.
- Schumacher HR Jr, Baker M, Lloyd E, et al. Febuxostat in the treatment of gout: 5-year findings of the FOCUS efficacy and safety study. Rheumatology 2009; 48:188–194.
- Reinders MK, van Roon EN, Jansen TL. Efficacy and tolerability of uratelowering drugs in gout: a randomised controlled trial of benzbromarone versus probenecid after failure of allopurinol. Ann Rheum Dis 2009; 68:51– 56.
- Perez-Ruiz F, Sundy J, Krishnan E, et al. Efficacy and safety of Lesinurad (RDEA594), a novel uricosuric agent, given in combination with allopurinol refractory gout patients: randomised, double-blind, placebo-controlled, phase 2b study. In: EULAR Conference Proceedings; abstract OPO111; 2011.
••A novel uricosuric agent. - Bleyer A, Hurt TC. Genetic factors associated with gout and hyperuricemia. Adv Chronic Kidney Dis 2006; 13:124–130.
- Cammalleri L, Malaguarnera M. Rasburicase represents a new tool for hyperuricemia in tumour lysis syndrome and in gout. Int J Med Sci 2007; 2:83–93.
- Schumacher HR, Chen LX. Newer therapeutic approaches: gout. Rheum Dis Clin North Am 2006; 32:235–244.
- Vogt B. Urate oxidase (rasburicase) for treatment of severe tophaceous gout. Nephrol Dial Transplant 2005; 20:431–433.
- Sherman MR, Saifer MGP, Perez-Ruiz F. PEG-uricase in the management of treatment-resistant gout and hyperuricemia. Adv Drug Deliv Rev 2008; 60:59–68.
- Sundy J, Baraf HSB, Yood RA, et al. Efficacy and tolerability of pegloticase for the treatment of chronic gout in patients refractory to conventional treatments. Two randomised trials. JAMA 2011; 306:711–720.
- Khanna PP, Perex-Ruiz F, Maranian P, Khanna D. Long term therapy for chronic gout results in clinically important improvements iyn the health-related quality of life: short form 36 is responsive to change in chronic gout. Rheumatology 2011; 50:740–745.
Papers of particular interest, published within the annual period of review, have been highlighted as:
• of special interest
•• of outstanding interest
Additional references related to this topic can also be found in the Current World Literature section in this issue (pp. 239–241).









0 komentar:
Posting Komentar